2025 Medical Billing Software for Small Business: Top 10 Picks
Medical billing software for small businesses has become an essential tool to streamline financial management and enhance operational efficiency. As healthcare providers navigate complex billing processes, the right software solution can significantly impact their ability to manage expenses, track projects, and generate accurate invoices. With the increasing demand for user-friendly and comprehensive billing platforms, small medical practices are seeking solutions that offer customizable features, cloud-based accessibility, and robust reporting capabilities.
The year 2025 brings forth a new era of medical billing software, incorporating cutting-edge technologies and innovative approaches to address the unique needs of small healthcare businesses. From AI-powered systems and blockchain integration to telehealth billing solutions and value-based care models, the landscape of medical billing is undergoing a transformation. This article explores the top 10 picks for medical billing software in 2025, highlighting key features such as multi-lingual support, automated reminders, and seamless integration with existing financial systems. By examining these advanced solutions, healthcare providers can make informed decisions to optimize their billing processes and improve overall financial performance.
AI-Powered Medical Billing: The Future of Healthcare Finance

Artificial Intelligence (AI) is transforming the healthcare industry, particularly in the realm of medical billing and revenue cycle management (RCM). As healthcare providers seek to streamline their financial processes and improve efficiency, AI-powered solutions are emerging as game-changers in the field.
Machine Learning in Coding
Machine learning algorithms are revolutionizing medical coding and billing processes. These advanced systems can automate the coding of medical procedures and the generation of bills, significantly reducing errors and speeding up the reimbursement process . By leveraging natural language processing (NLP) techniques, AI can extract and organize information from Electronic Health Records (EHRs), making it easier for clinicians to access and interpret patient data .
One of the most significant applications of AI in medical billing is automated coding. Advanced NLP algorithms can analyze clinical documentation and automatically assign appropriate ICD-10 and CPT codes with a high degree of accuracy . This not only accelerates the coding process but also minimizes the likelihood of human error, leading to fewer claim denials and faster reimbursements.
Predictive Analytics for Claim Denials
Claim denials present a significant financial risk for healthcare providers. According to Change Healthcare, initial claim denials totaled $262 billion out of $3 trillion in claims submitted in 2016, putting as much as 3.3 percent of net patient revenue at risk . However, AI-powered predictive analytics is revolutionizing denial management.
Machine learning algorithms can analyze vast amounts of historical billing data to identify patterns that lead to denials and flag potential issues before claims are submitted . This proactive approach significantly reduces the administrative burden of managing denied claims and improves cash flow for healthcare providers.
For example, RCCH Healthcare Partners implemented a predictive analytics solution that categorized denials into high-value, mid-range, and low-value categories. This implementation resulted in an 18 percent improvement in accounts receivable (A/R) days and a 30 percent increase in collections .
AI-Assisted Patient Inquiries
AI is also enhancing patient communication and satisfaction in the billing process. AI-powered chatbots and virtual assistants are increasingly being used to handle routine billing inquiries from patients . These systems can provide instant responses to common questions about bills, insurance coverage, and payment options, improving patient satisfaction and reducing the workload on billing staff.
As we look towards 2025, it’s clear that AI will play an integral role in addressing pressing revenue cycle management issues, including prior authorizations, claim status checks, and out-of-pocket cost estimates . With the potential to automate up to 60% of claims processing by 2025, AI promises faster processing, increased accuracy, and an enhanced customer experience in medical billing .
Blockchain Technology in Medical Billing

Blockchain technology, originally developed for cryptocurrencies, is emerging as a game-changer in the medical billing landscape. This innovative approach addresses some of the most pressing challenges in healthcare finance, particularly in terms of security, transparency, and efficiency . By leveraging blockchain technology, healthcare providers can streamline billing processes, enhance data security, and improve overall efficiency .
Secure Transaction Records
One of the primary applications of blockchain in medical billing is creating a secure and immutable record of transactions. Each billing transaction, from the initial service provision to the final payment, can be recorded as a “block” in the chain. This creates an unalterable audit trail that can significantly reduce fraud and disputes . The decentralized and cryptographic nature of blockchain provides a secure platform for storing and sharing sensitive medical information. Each transaction is encrypted and linked to the previous one, creating a chain that is difficult to alter without consensus from the network, ensuring the integrity and security of the data .
Smart Contracts for Automated Billing
Smart contracts, a feature of blockchain technology, are being implemented to automate many aspects of the billing process. These self-executing contracts with the terms of the agreement directly written into code can automatically trigger actions such as claim submission, payment processing, and even the application of contractual discounts . This automation not only speeds up the billing cycle but also reduces the potential for human error and improves the consistency of billing practices. By automating billing processes through smart contracts, healthcare providers can reduce administrative costs and the need for manual intervention .
Enhanced Data Privacy
Blockchain technology is enhancing patient privacy and data security. Unlike traditional centralized databases, which can be vulnerable to large-scale data breaches, blockchain’s decentralized nature makes it much more difficult for unauthorized parties to access or tamper with sensitive information . Patients can have greater control over their data, granting and revoking access as needed. Blockchain-enabled systems and software can streamline patient consent management for data sharing. Patients can set conditions for using and sharing their data through smart contracts. These contracts automatically enforce consent agreements, making the process more efficient and less prone to errors .
In the evolving landscape of medical billing, companies like Wenour are at the forefront of implementing blockchain solutions. By leveraging this technology, Wenour helps healthcare providers enhance data security, streamline billing processes, and improve overall financial performance. As blockchain continues to revolutionize medical billing, it promises to create a more efficient, transparent, and secure healthcare financial ecosystem.
Telehealth and Remote Patient Monitoring Billing

The landscape of telehealth and remote patient monitoring (RPM) billing has undergone significant changes, particularly in light of the COVID-19 public health emergency (PHE). Healthcare providers and billing specialists need to stay informed about the evolving reimbursement policies and coding requirements to ensure proper compensation for these services.
New Billing Codes for Virtual Care
The Centers for Medicare & Medicaid Services (CMS) has introduced several new codes to accommodate the growing demand for virtual care services. For instance, CMS has proposed three new “Advanced Primary Care Management” HCPCS codes that focus on interactions with patients at their preferred time and location . These codes, GPCM1, GPCM2, and GPCM3, provide reimbursement for advanced primary care management services using clinical staff under the direction of a physician or other qualified healthcare professional .
In addition, CMS has proposed new codes for digital mental health treatment devices. These include GMBT1 for the supply and initial education of digital mental health treatment devices, and GMBT2 and GMBT3 for monthly treatment management services related to the patient’s use of these devices .
Reimbursement Policies for Telehealth
CMS has implemented several changes to telehealth reimbursement policies. Notably, the agency has proposed permanent coverage of two-way, real-time, audio-only telehealth services for beneficiaries in their homes when video technology is not available or not consented to by the patient . This change aims to increase access to care, especially for patients who may have technological limitations.
Furthermore, CMS has extended the definition of “direct supervision” to include access by audio-video telemedicine, rather than requiring physical presence in the same room . This modification allows for greater flexibility in providing supervised care.
Challenges in Cross-State Billing
One of the ongoing challenges in telehealth billing is navigating the complexities of cross-state services. Laws regarding physician licensure continue to defer to state regulations, with no overarching federal policy in place . This situation can create difficulties for healthcare providers offering telehealth services across state lines, as they must ensure compliance with varying state regulations.
In the evolving landscape of telehealth and RPM billing, companies like Wenour are at the forefront of helping healthcare providers navigate these complexities. By staying up-to-date with the latest billing codes and reimbursement policies, Wenour assists medical practices in optimizing their revenue cycle management for telehealth services.
As the healthcare industry continues to adapt to the increased demand for virtual care, it’s crucial for providers to stay informed about these billing changes and work with experienced medical billing partners to ensure accurate reimbursement for telehealth and RPM services.
Value-Based Care and Its Impact on Billing

Value-based care has transformed the healthcare landscape, significantly impacting medical billing practices. This shift from fee-for-service to outcome-based reimbursement has led to new payment models and quality metrics that healthcare providers must navigate.
Quality Metrics in Billing
The Centers for Medicare & Medicaid Services (CMS) has introduced several initiatives to promote quality-driven care. One such initiative is the MIPS Value Pathways (MVPs), which aim to increase specialist engagement in value-based care . CMS has proposed six new MVPs, including ophthalmology, dermatology, and pulmonology, to expand the program’s reach .
To further incentivize quality care, CMS has proposed a Complex Organization Adjustment for virtual groups and APM Entities starting in 2025 . This adjustment awards achievement points for each electronic Clinical Quality Measure (eCQM) meeting specific criteria, supporting organizational complexity while maintaining quality standards.
Bundled Payments and Episodes of Care
Bundled payment arrangements have become a popular method for embracing value-based care without fully exposing providers to downside financial risk . Under this model, providers receive a single payment for all services related to a specific episode of care. If the cost of care is less than the bundled payment, providers keep the difference; if it’s more, they bear the loss .
CMS has developed several bundled payment models, including the Medicare Bundled Payment for Care Improvement (BCPI) Advanced Model and the Comprehensive Care for Joint Replacement (CJR) Model . These models aim to improve care coordination and reduce unnecessary costs.
Risk-Sharing Arrangements
Risk-sharing arrangements are becoming increasingly common in value-based care models. CMS is proposing to allow eligible Accountable Care Organizations (ACOs) with a successful track record to access prepaid shared savings . This advance on earned savings encourages investment in staffing, healthcare infrastructure, and additional services for Medicare beneficiaries.
To promote health equity, CMS is also proposing a health equity benchmark adjustment for ACOs serving rural and underserved communities . This adjustment, similar to the one in the Innovation Center’s ACO REACH Model, has been associated with increased safety net provider participation.
In the evolving landscape of value-based care, companies like Wenour are at the forefront of helping healthcare providers navigate these complex billing changes. By staying informed about new payment models and quality metrics, Wenour assists medical practices in optimizing their revenue cycle management while delivering high-quality, patient-centered care.
Interoperability and Data Sharing in Medical Billing

FHIR Standards for Data Exchange
Fast Healthcare Interoperability Resources (FHIR) has emerged as a crucial standard for addressing data exchange challenges in healthcare. FHIR’s modular and resource-oriented architecture promotes clinical interoperability among disparate systems, enabling electronic health records, medical apps, and other health-related platforms to seamlessly exchange data . This standardization ensures a unified view of patient information, fostering patient-centric care and informed decision-making.
FHIR utilizes a RESTful API architecture, simplifying the development process for healthcare applications. This web-friendly design enhances interoperability, making health data easily accessible and shareable across various platforms . The adoption of FHIR standards facilitates the exchange of patient information between different EHR systems, ensuring healthcare professionals have access to comprehensive and up-to-date patient records, regardless of the EHR platform used .
Real-Time Eligibility Verification
Real-time eligibility verification has transformed the insurance verification process in healthcare settings. This technology allows for instant verification of patient insurance coverage, reducing the risk of claim denials and accelerating the billing process . By providing real-time access to patient data, automated insurance verification services ensure that healthcare providers have the most up-to-date and accurate information regarding insurance coverage and benefits .
The integration of these services with hospital information systems and electronic health records enhances workflow efficiency, minimizes administrative burdens, and fosters a more organized and productive environment . Real-time eligibility verification also improves patient satisfaction by reducing financial anxiety, avoiding surprise bills, and increasing transparency in costs .
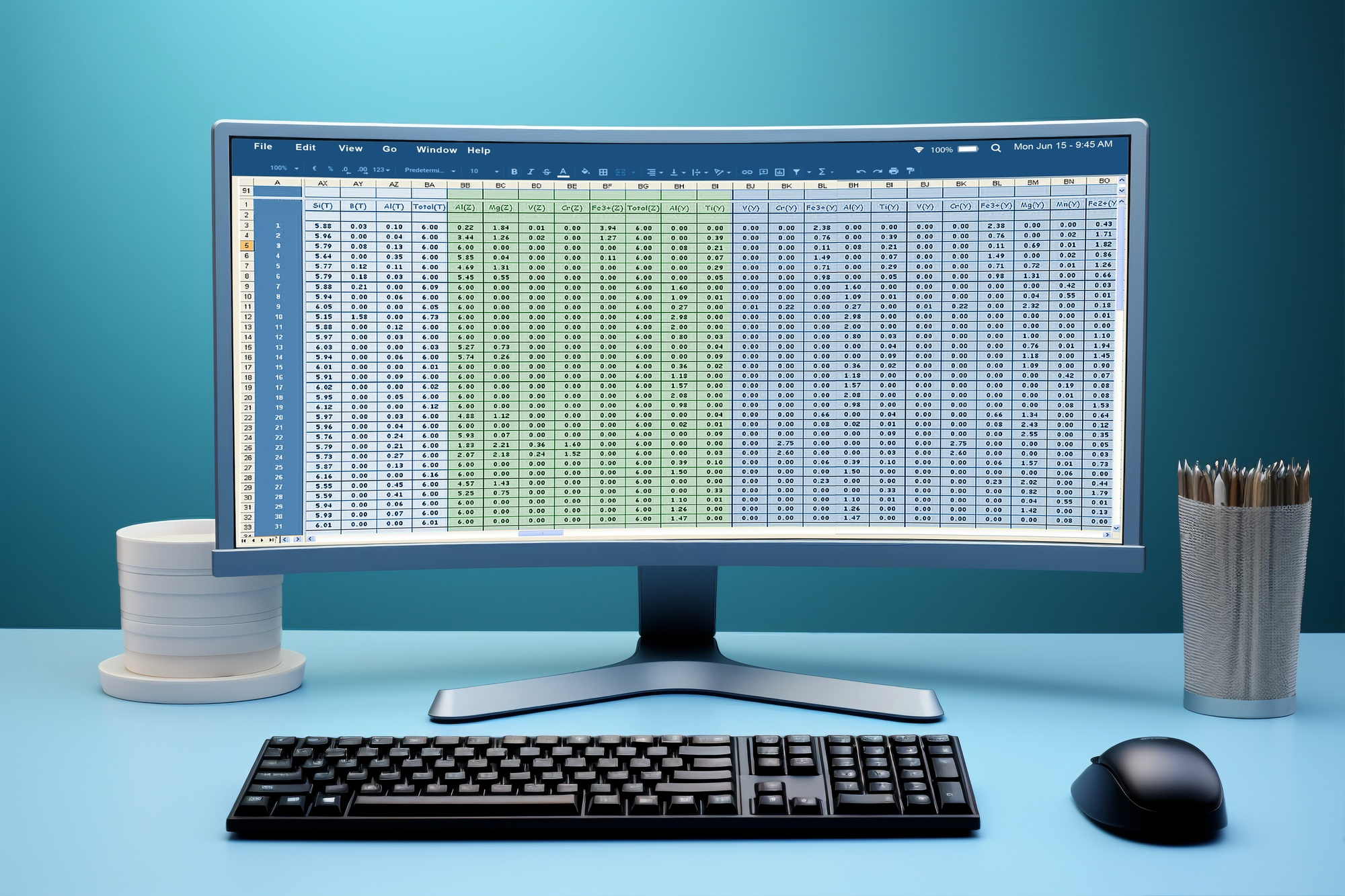
Improved Claims Processing Efficiency
Artificial intelligence (AI) continues to play a pivotal role in revolutionizing claims processing software. AI-powered automation solutions streamline workflows, reduce manual intervention, and improve efficiency throughout the claims lifecycle . These algorithms automate routine tasks such as data entry, document processing, and claims triaging, enabling insurers to process claims faster, minimize errors, and allocate resources more effectively .
Natural language processing (NLP) technologies enable claims processing software to understand and extract information from unstructured text data, such as claim notes, emails, and customer correspondence . By analyzing large volumes of textual data efficiently, NLP algorithms identify key insights, detect patterns, and make data-driven decisions, leading to improved accuracy and faster processing times in claims processing .
In the evolving landscape of medical billing, companies like Wenour are at the forefront of implementing these advanced technologies. By leveraging FHIR standards, real-time eligibility verification, and AI-powered claims processing, Wenour helps healthcare providers optimize their revenue cycle management, reduce errors, and improve overall financial performance.
Conclusion
The evolution of medical billing software for small businesses in 2025 has a significant impact on healthcare finance management. From AI-powered solutions to blockchain integration, these advancements streamline processes, enhance security, and improve overall efficiency. The shift towards value-based care models and the growing importance of telehealth services further shape the landscape, requiring healthcare providers to adapt their billing practices. Wenour’s medical billing services are at the forefront of implementing these innovative technologies, helping practices navigate the complexities of modern healthcare finance.
As the healthcare industry continues to evolve, the importance of interoperability and data sharing in medical billing becomes increasingly evident. The adoption of FHIR standards, real-time eligibility verification, and AI-powered claims processing contribute to a more connected and efficient healthcare ecosystem. To wrap up, these advancements in medical billing software offer small healthcare businesses the tools to optimize their financial performance and focus on delivering high-quality patient care. Explore Wenour’s Medical Billing Services to enhance your practice’s financial management and stay ahead in the ever-changing healthcare landscape.
FAQs
What are the top medical billing software options for 2024? The most highly regarded medical billing software for 2024 includes DrChrono, which is best overall; Kareo Billing, which is ideal for small practices; CureMD, recommended for large practices; AdvancedMD, which features the best patient portal; and CentralReach, which is the top choice for behavior therapists.
How is the medical billing outsourcing market expected to grow? The global medical billing outsourcing market was valued at approximately USD 14.65 billion in 2023. It is anticipated to increase to USD 16.32 billion in 2024 and further expand to USD 39.98 billion by 2032, with a compound annual growth rate (CAGR) of 11.8% from 2024 to 2032.
What are some of the best software options for general billing purposes? For general billing, the top free software options include Wave, which is great for growing businesses; PayPal, a well-known option; Zoho Invoice, which includes a mini-CRM; Square, suitable for in-person sales; Bookipi, a straightforward invoicing solution; and Paymo, which is excellent for time-based invoicing.
Is it beneficial to start a medical billing company? Starting a medical billing company can be a lucrative venture due to the increasing demand for these services. It is crucial, however, to ensure that professional services are used for essential back-end processes such as insurance coverage, legal advice, and accounting to support the business effectively.