Medical Billing: Understanding Improtant 2024 Statistics on Claim Denials and Appeals in the USA

In the complex world of healthcare, medical billing plays a crucial role in ensuring the financial viability of medical practices and hospitals. However, the process is often fraught with challenges, with claim denials and appeals being a major concern for both healthcare providers and patients. Understanding the statistics and trends surrounding medical claim denials and appeals is essential for navigating the intricacies of medical billing. In this comprehensive guide, we will delve into the topic, providing insights into the reasons behind claim denials, the appeal process, and the impact on patients and healthcare providers.
Table of Contents
- Introduction
- Overview of Medical Billing
- The Importance of Claim Denials and Appeals
Statistics on Claim Denials in the USA
- Denial Rates by Insurers
- Denial Rates by State
- Denial Rates by Plan Metal Levels
Reasons for Claim Denials
- Lack of Prior Authorization or Referral
- Out-of-Network Provider
- Excluded Services
- Medical Necessity
- Other Reasons
The Appeal Process
- Internal Appeals
- External Appeals
Challenges Faced by Patients
- Financial Impact
- Barriers to Appealing Denials
Impact on Healthcare Providers
- Revenue Loss
- Administrative Burden
The Role of the Affordable Care Act (ACA)
- Transparency Data Reporting
- Monitoring Denials
Proposed Solutions and Reforms
- Enhanced Data Collection and Reporting
- Strengthening Oversight and Enforcement
The Role of Medical Billing Outsourcing
- Introduction to Wenour: Remote Medical Billing Services in the USA
- Benefits of Outsourcing Medical Billing
- Conclusion
1. Introduction
The healthcare landscape in the USA is constantly evolving, and with it, the complexities of medical billing. Claim denials have become increasingly prevalent, causing frustration and financial strain for both patients and healthcare providers. To address this issue, it is crucial to understand the underlying reasons for claim denials, the appeal process, and potential solutions. This guide aims to provide a comprehensive overview of medical claim denials and appeals, shedding light on the statistics, challenges, and potential reforms.
2. Overview of Medical Billing
Before diving into the specifics of claim denials and appeals, let’s first establish a foundational understanding of medical billing. Medical billing is the process of submitting and following up on claims with health insurance companies to receive payment for services provided by healthcare providers. It involves translating medical procedures, diagnoses, and treatments into standardized codes for billing purposes. Accurate and timely billing is essential for healthcare providers to receive reimbursement for their services and ensure financial stability.
3. The Importance of Claim Denials and Appeals
Claim denials can have significant financial implications for both patients and healthcare providers. For patients, denied claims may result in unexpected out-of-pocket expenses, leading to financial strain and potential delays in receiving necessary medical care. Healthcare providers, on the other hand, face revenue loss and increased administrative burden when claims are denied. The appeal process becomes crucial in rectifying these denials, but it often entails additional time, effort, and resources.
4. Statistics on Claim Denials in the USA
To gain a deeper understanding of the prevalence and impact of claim denials, let’s explore some statistics. These statistics provide valuable insights into denial rates across insurers, states, and plan metal levels.
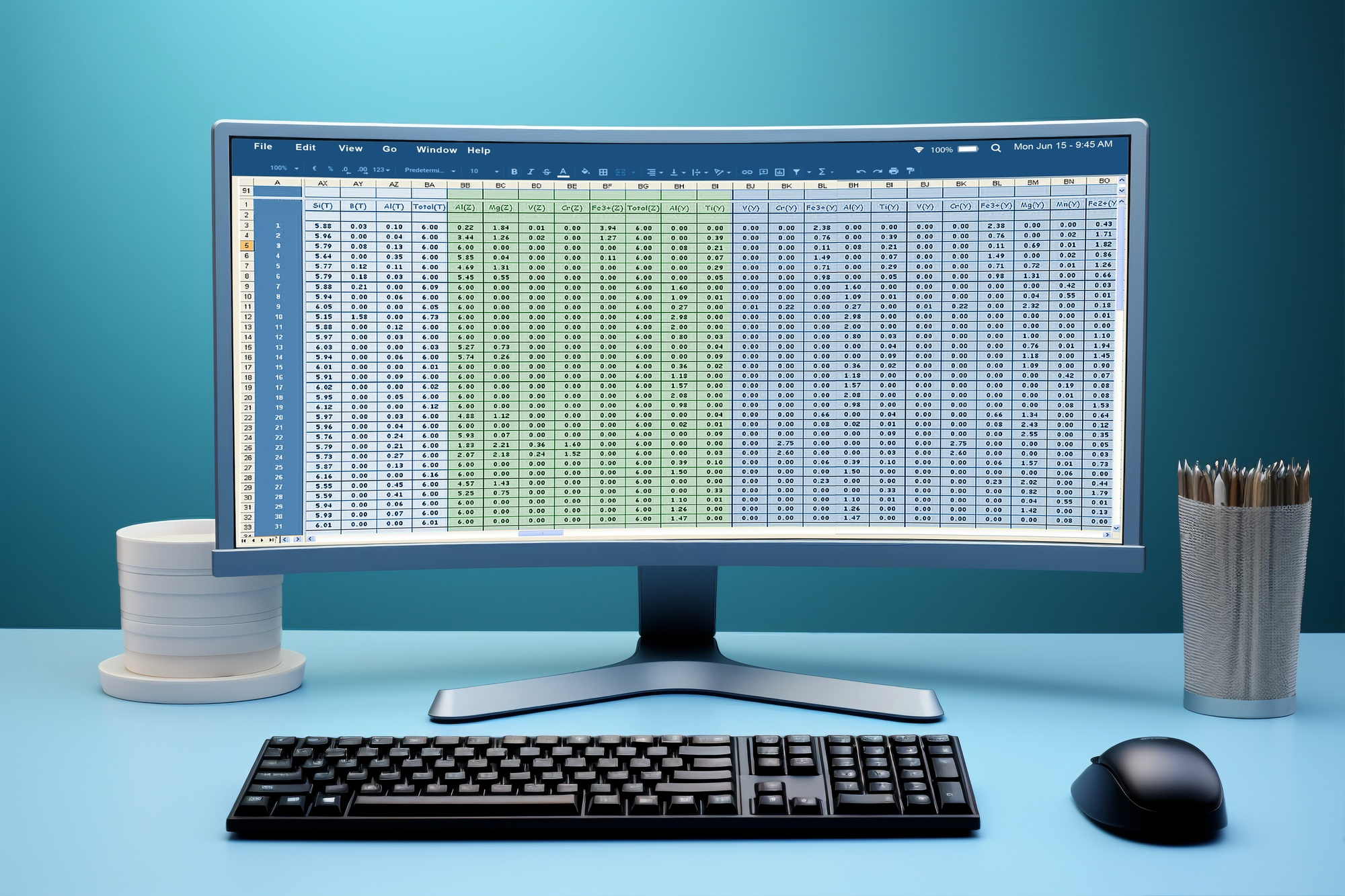
Denial Rates by Insurers
According to data from the Centers for Medicare and Medicaid Services (CMS), denial rates for in-network claims varied widely among HealthCare.gov insurers in 2021. On average, nearly 17% of in-network claims were denied. However, denial rates ranged from as low as 2% to as high as 49%. Some insurers consistently reported high denial rates, such as Meridian Health Plan of Michigan, Absolute Total Care in South Carolina, and Celtic Insurance in multiple states.
Denial Rates by State
Denial rates also exhibited variations at the state level. For example, in Florida, the average denial rate for in-network claims in 2021 was 13%. However, when examining specific insurers within the state, denial rates ranged from 15% to 42%. This disparity highlights the importance of understanding denial rates within specific geographic regions.
Denial Rates by Plan Metal Levels
Plan metal levels, such as bronze, silver, gold, platinum, and catastrophic, also play a role in denial rates. On average, HealthCare.gov issuers denied 15.9% of in-network claims in bronze plans, 17.3% in silver plans, 17.1% in gold plans, 11.4% in platinum plans, and 19.7% in catastrophic plans. These variations underscore the need for patients to carefully consider plan options when selecting their coverage.
5. Reasons for Claim Denials
Understanding the reasons behind claim denials is crucial for addressing and minimizing their occurrence. Let’s explore the common reasons cited by insurers for denying claims.
Lack of Prior Authorization or Referral
One common reason for claim denials is the lack of prior authorization or referral. Insurers often require preapproval for certain procedures or specialist visits. Failure to obtain the necessary authorization or referral can result in claim denials. It is important for patients and healthcare providers to familiarize themselves with their insurance plan’s requirements to avoid potential denials.
Out-of-Network Provider
Another reason for claim denials is seeking care from an out-of-network provider. Insurance plans typically have networks of preferred providers, and seeking care from providers outside of these networks may lead to denials. Patients should ensure that their chosen healthcare providers are in-network to minimize the risk of claim denials.
Excluded Services
Some services may be excluded from coverage under certain insurance plans. If a claim is submitted for an excluded service, it is likely to be denied. Patients should review their insurance plan documents to understand which services are covered and which are excluded to avoid potential denials.
Medical Necessity
Claims may also be denied based on the insurer’s assessment of medical necessity. Insurers evaluate whether a specific treatment or service is deemed medically necessary based on established criteria. If the insurer determines that the service is not medically necessary, the claim may be denied. This can be particularly challenging, as medical necessity criteria may vary among different insurers.
Other Reasons
The category of “all other reasons” encompasses a wide range of potential causes for claim denials. This catch-all category often includes administrative errors, missing documentation, coding discrepancies, and other factors that lead to claim denials. It is important for healthcare providers to ensure accurate and complete documentation to minimize the risk of denials.
6. The Appeal Process
When a claim is denied, patients and healthcare providers have the option to appeal the decision. Understanding the appeal process is crucial for navigating the system effectively. Let’s explore the two main types of appeals: internal appeals and external appeals.
Internal Appeals
Internal appeals involve challenging the denial decision within the insurance company. Patients or their designated representatives can submit a written appeal, providing additional documentation, medical records, or other supporting evidence to contest the denial. It is essential to carefully follow the insurer’s guidelines and deadlines for submitting internal appeals.
External Appeals
If the internal appeal is unsuccessful or not available, patients may have the option to pursue an external appeal. External appeals involve seeking an independent review of the denial decision by a third-party organization. The rules and eligibility criteria for external appeals vary by state and type of insurance plan. Patients should consult their insurance plan documents or contact their state insurance department to determine if they are eligible for an external appeal.
7. Challenges Faced by Patients
Claim denials can have a significant impact on patients, both financially and emotionally. Let’s explore some of the challenges faced by patients when dealing with denials.
Financial Impact
Denied claims can result in unexpected out-of-pocket expenses for patients. This financial burden can be particularly challenging for individuals facing chronic illnesses or high-cost treatments. Patients may be forced to delay or forgo necessary medical care due to the financial strain caused by denied claims.
Barriers to Appealing Denials
The appeal process can be complex and time-consuming, posing challenges for patients. Many individuals lack the knowledge and resources to navigate the appeals system effectively. Additionally, some patients may face language barriers or limited access to support services, further hindering their ability to appeal denials.
8. Impact on Healthcare Providers
Claim denials not only affect patients but also have a significant impact on healthcare providers. Let’s explore the challenges faced by healthcare providers as a result of claim denials.
Revenue Loss
When claims are denied, healthcare providers face revenue loss. Unpaid claims can have a substantial financial impact, especially for smaller practices or healthcare facilities operating on tight budgets. The need to resubmit denied claims and navigate the appeals process can result in delayed or reduced payments, further straining the financial viability of healthcare providers.
Administrative Burden
The appeal process places an additional administrative burden on healthcare providers. Staff members must allocate time and resources to gather necessary documentation, prepare appeals, and navigate the complex appeals system. This diversion of resources can impact the efficiency and productivity of healthcare providers, potentially affecting patient care.
9. The Role of the Affordable Care Act (ACA)
The Affordable Care Act (ACA) introduced provisions aimed at improving transparency and reducing claim denials. Let’s explore the role of the ACA in addressing this issue.
Transparency Data Reporting
The ACA requires transparency data reporting by all non-grandfathered employer-sponsored health plans and non-group plans sold on and off the marketplace. Insurers are required to report data on claims payment policies, enrollment, disenrollment, denial rates, rating practices, and other relevant information. Transparency data aims to inform regulators and consumers about how health plans operate in practice.
Monitoring Denials
The ACA tasked the Department of Health and Human Services (HHS) with monitoring denials by health plans on the Obamacare marketplace, as well as those offered through employers and insurers. The collection and analysis of denial data are essential for identifying trends, ensuring compliance with the ACA, and developing strategies to mitigate denials.
10. Proposed Solutions and Reforms
To address the challenges posed by claim denials, various solutions and reforms have been proposed. Let’s explore some potential strategies for reducing denials and improving the appeals process.
Enhanced Data Collection and Reporting
To gain a comprehensive understanding of denial trends, there is a need for enhanced data collection and reporting. This includes expanding the data collected under the ACA to encompass a broader range of fields, such as out-of-network claims and specific reasons for denials. By collecting and analyzing more detailed data, policymakers and regulators can identify patterns and develop targeted interventions.
Strengthening Oversight and Enforcement
To ensure compliance with the ACA and minimize inappropriate denials, there is a need for strengthened oversight and enforcement mechanisms. This includes conducting audits to verify the accuracy and consistency of reported data and implementing penalties for non-compliance. By holding insurers accountable, regulators can incentivize fair and transparent claims processing.
11. The Role of Medical Billing Outsourcing
In the realm of medical billing, outsourcing has emerged as a viable solution for healthcare providers seeking to optimize revenue cycle management. One such company, Wenour, provides remote medical billing services in the USA. While not directly related to claim denials and appeals, outsourcing medical billing can indirectly contribute to reducing denials by ensuring accurate and timely billing processes.
Introduction to Wenour: Remote Medical Billing Services in the USA
Wenour is a trusted provider of remote medical billing services in the USA. Their team of experienced medical billing professionals handles the entire billing process, from claim submission to follow-up and appeals. By outsourcing medical billing to Wenour, healthcare providers can streamline their revenue cycle management, reduce administrative burdens, and improve the accuracy and efficiency of their billing processes.
Benefits of Outsourcing Medical Billing
Outsourcing medical billing offers several benefits for healthcare providers. It allows them to focus on delivering quality patient care while entrusting billing tasks to experts in the field. Wenour’s team ensures adherence to coding guidelines, stays updated with industry changes, and employs efficient billing practices, thereby minimizing the risk of denials. By leveraging the expertise of Wenour, healthcare providers can optimize their revenue cycle and enhance their financial stability.
12. Conclusion
Medical billing is a complex process, and claim denials and appeals are significant challenges within the healthcare industry. Understanding the statistics, reasons, and impact of claim denials is crucial for patients and healthcare providers alike. By advocating for enhanced data collection, strengthening oversight and enforcement, and considering solutions like medical billing outsourcing, stakeholders can work towards reducing denials and improving the appeals process. Ultimately, the goal is to ensure fair and transparent billing practices, providing patients with access to the care they need while supporting the financial viability of healthcare providers.
In the ever-evolving landscape of medical billing, staying informed and proactive is key. By addressing the challenges surrounding claim denials and appeals, we can strive for a more efficient and patient-centered healthcare system.