How to Handle Denied Family Practice Claims in Legacy AR Systems

This article delves into the best practices for managing denied family practice claims in the context of legacy accounts receivable (AR) systems. It explores setting up a strategic denial management framework, which includes conducting a thorough root cause analysis to prevent future denials, and highlights the pivotal role of revenue cycle management in sustaining a practice’s financial health. Additionally, it provides practical insights into implementing denial management processes that leverage the power of intelligent automation to enhance efficiency. By emphasizing the importance of authorization, accurate medical billing, and coding, this article aims to guide healthcare providers through the meticulous process of handling insurance claims and improving the management of claim files to dodge the pitfalls of underpayments and overpayments, ultimately securing the financial foundation of healthcare practices.
Setting Up a Denial Management Strategy
Importance of Denial Management
Denial management in medical billing is crucial as it directly impacts the financial stability of healthcare providers. Effective denial management not only resolves existing claim denials but also prevents future ones, optimizing cash flow. By reducing the denial rate, healthcare providers can ensure a steady revenue stream, essential for maintaining operational efficiency and quality patient care.
Key Components of a Strategy
A robust denial management strategy involves several key components:
- Identification of Denials: The first step is to accurately identify the reasons behind claim denials. This involves interpreting payer feedback and using claim adjustment reason codes (CARC) to pinpoint the exact issues.
- Resolution and Appeals: Once the reasons for denials are identified, the next step involves appealing denied claims to ensure they are paid. This requires a systematic approach to manage, monitor, and prevent future denials.
- Preventive Measures: Preventing denials from occurring is a crucial strategy. This includes training staff, adjusting workflows, and revising processes based on insights gathered from previous denials.
- Technology and Automation: Implementing technology solutions, such as automated verification tools and advanced data analytics, can significantly reduce the occurrence of denials by catching common errors and ensuring compliance with payer policies.
- Collaborative Efforts: Engaging all departments within the healthcare organization to work together can enhance the overall effectiveness of the denial management strategy. This collaborative approach ensures that everyone understands their role in reducing denials and improving the revenue cycle.
By focusing on these components, healthcare providers can develop a comprehensive strategy that not only addresses current denials but also minimizes future occurrences, thereby enhancing financial outcomes and patient satisfaction. Additionally, leveraging the expertise of specialized medical billing companies like Wenour can further streamline the process, ensuring that claims are managed efficiently and effectively.
Implementing Denial Management Processes
Automated Tools for Claims Denials
Implementing automated tools significantly enhances the efficiency and accuracy of denial management processes. By utilizing sophisticated algorithms and machine learning, these systems proactively identify and rectify errors before claims are submitted, dramatically reducing denial rates. Automated healthcare denials management systems categorize denials based on their likelihood of successful appeal, allowing healthcare organizations to focus on the most recoverable revenues. This strategic approach not only speeds up the reimbursement process but also contributes to a more effective allocation of resources.
Training Your Denial Management Team
Equipping the revenue cycle staff with the necessary skills to manage denials effectively is crucial. Ongoing training ensures that the team is proficient in using advanced tools and understands the best practices for denial prevention. This includes learning how to conduct detailed denial analysis, recognizing the common causes of denials, and implementing solutions to prevent future issues. Moreover, fostering a culture of continuous improvement and knowledge sharing across the team can lead to more sustainable denial management strategies, significantly reducing the occurrence of claim rejections and denials.
Managing Denied Claims in Legacy AR Systems
Handling Outdated Technology
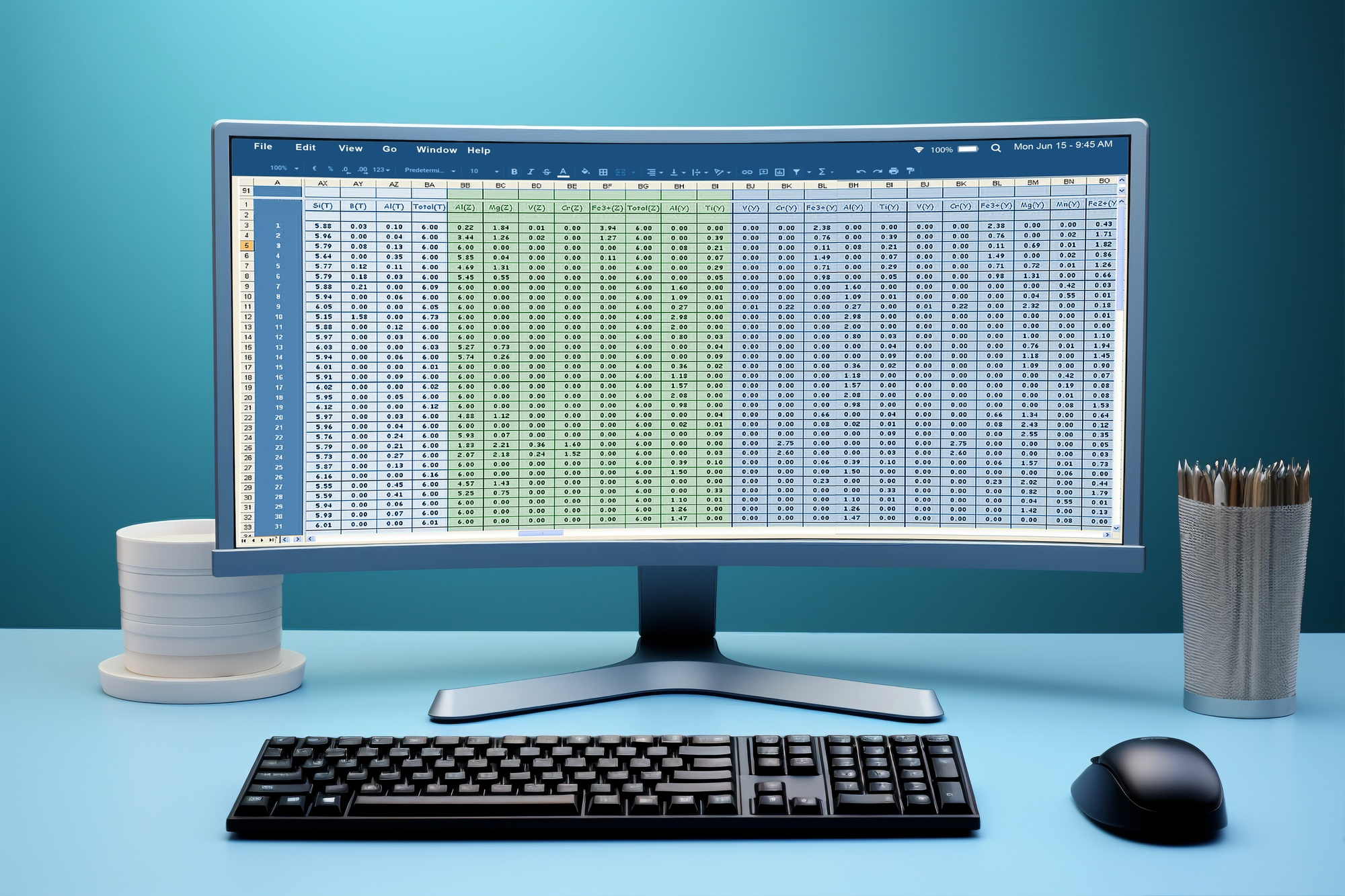
Managing denied claims in legacy accounts receivable systems often involves dealing with outdated technology, which can significantly hinder the efficiency of medical billing processes. A staggering 33% of healthcare organizations rely on antiquated systems that are not equipped to handle modern claim processing demands, leading to increased denials and prolonged revenue cycles. To combat this, it is crucial for practices to consider upgrading their technology. Implementing more current systems can reduce the occurrence of errors and streamline the claims process. Companies like Wenour specialize in providing cutting-edge medical billing solutions that can seamlessly integrate with existing systems, enhancing overall efficiency and reducing the burden of legacy technology.
Best Practices for Efficient Management
Effective management of denied claims within legacy AR systems requires meticulous attention to detail and a proactive approach. Regular audits are essential, as they help identify and rectify discrepancies that lead to denials. Additionally, maintaining accurate and detailed documentation is crucial. This includes ensuring that all claim forms are filled out correctly and that every service provided is properly coded and documented. Implementing electronic health records (EHR) and utilizing revenue cycle management software can further aid in minimizing errors and improving the accuracy of claims submissions. Moreover, engaging a specialized medical billing firm like Wenour can provide the expertise needed to navigate the complexities of legacy systems, ensuring that claims are processed efficiently and effectively.
Preventing Future Denials
Root Cause Analysis
To effectively prevent future denials, healthcare providers must conduct a thorough root cause analysis (RCA) for each denial, identifying the underlying reasons and addressing them directly. This process involves not only relying on the reason codes provided by payers but also conducting an internal analysis of the medical record, charges, and the billed claim to determine potential root causes. By understanding and acting on these specific causes, healthcare providers can implement targeted corrective actions, reducing the occurrence and reoccurrence of denials.
Staff Training and Workflow Changes
Regular training and education of staff on coding guidelines, payer requirements, and changes in healthcare regulations are crucial to minimize errors that lead to denials. Additionally, enhancing documentation practices ensures comprehensive and clear records, which aid in faster denial appeals and reduce billing discrepancies. Healthcare organizations should also continuously evaluate their internal workflows to identify areas for improvement, ensuring that all staff members are up to speed with the latest procedures and compliance requirements. Implementing automated tools for insurance verification can further reduce errors and expedite the medical billing denial management process efficiently.
By fostering effective communication between billing and clinical staff, healthcare providers can address denial issues promptly and collaboratively, ensuring a knowledgeable team adept at handling complex reimbursement challenges. Moreover, engaging a specialized medical billing firm like Wenour can provide the expertise needed to navigate the complexities of legacy systems, ensuring that claims are processed efficiently and effectively.
Conclusion
Navigating the complexities of denied family practice claims within legacy AR systems is essential for maintaining financial stability and ensuring the continuity of quality patient care. This article has highlighted the importance of deploying a structured denial management strategy, focusing on identifying reasons behind denials, implementing preventive measures through training and technology, and the value of regular audits. Furthermore, the integration of automated tools and collaborative efforts across departments underscores a proactive approach to minimizing error rates and enhancing the efficiency of claim processing. Engaging with specialized medical billing companies like Wenour plays a pivotal role in this process, offering expertise and sophisticated solutions that can seamlessly integrate with existing systems to optimize billing operations and financial outcomes.
In conclusion, the road to mitigating the effects of denied claims and underpayments in the realm of healthcare requires a blend of strategic, analytical, and technological efforts. By conducting thorough root cause analysis, continuously training staff, and adopting advanced technological solutions, healthcare providers can significantly reduce the frequency and impact of denials. Partnering with experienced medical billing firms such as Wenour not only provides the necessary support and resources needed for effective denial management but also ensures a streamlined, efficient billing process that is essential for the sustainability and growth of healthcare practices in today’s challenging environment.
FAQs
What steps can be taken if a claim is denied? If your claim is denied and you believe this to be incorrect, you can appeal the decision. This process involves sending a detailed written request to the insurance company, explaining why the claim should be approved. Additionally, you might have the opportunity to argue your case before an independent review board.
What are common reasons for a claim to be denied? Claim denials typically occur due to process errors or issues with coverage. Other reasons include services being deemed not appropriate or not authorized.
How can you address denials based on medical necessity? To contest a denial due to medical necessity, you should prepare a detailed letter, possibly written by you or your healthcare provider. This letter should clearly state why the denial was incorrect, including all relevant details and evidence. Make sure to include your name, claim number, and health insurance member number in the letter.
What distinguishes a rejected claim from a denied claim? A rejected claim is one that is not processed due to incorrect data input and occurs before any claim processing. In contrast, a denied claim refers to one that has been processed but is deemed unpayable based on the terms of the patient-payer contract or other reasons identified during the processing phase.