The Artificial Intelligence Advantage: Addressing Healthcare Denials Management and Revenue Integrity
Table of contents
• Introduction
• The Rising Denial Problem in Healthcare
• The Role of Artificial Intelligence (AI) in Denials Management
• Preventing Denials with AI-driven Analytics
• Conclusion
Introduction
Hey there, fellow humans! Let’s talk about the rising denial problem in the healthcare industry. *Gasp* Apparently, hospitals have been experiencing an increase in payment denials, and it doesn’t look pretty. According to a recent survey, a whopping 89% of healthcare providers reported an increase in denials between 2017 and 2020. And it gets worse! Half of them even experienced a ‘significant’ increase in denials. Yikes!
Statistics on denial rates
And here’s the cherry on top: Medicare Advantage plans seem to be leading the denial parade. A survey found that the initial inpatient level of care claim denial rate for these plans was a staggering 5.8% compared to 3.7% for all other payers. Talk about a tough crowd to please!
Challenges in applying correct patient status
So, what’s causing all these denials? Well, it seems like there are two main challenges. First, there’s considerable subjectivity in how physicians and case managers determine the appropriate patient status. It’s like they’re playing a never-ending game of “guess the status” with outdated information! And second, different payers have their own unique set of criteria. It’s like having to solve a new puzzle for each payer. Can someone say “tedious”?
The financial impact on healthcare organizations
Denials don’t just sting the providers, they also affect the financial sustainability of healthcare organizations. In 2022, hospitals had to write off a whopping 5.9% of their inpatient revenue as uncollectible. Ouch! That’s like throwing money down the drain. And with the denial rate constantly on the rise, it’s becoming a real headache for these organizations.
Next up, let’s talk about how Artificial Intelligence (AI) swoops in to save the day by addressing these denial issues and improving revenue integrity. Stay tuned, folks!
The Rising Denial Problem in Healthcare
Ah, denials. The bane of every healthcare organization’s existence. It’s like playing a game of Whack-a-Mole, except instead of moles, you’re dealing with denial after denial. Fun, right?
Let’s talk about the staggering statistics on denial rates first. According to a recent industry survey, Medicare Advantage plans have an initial inpatient level of care claim denial rate of 5.8%, while all other payer categories have a comparatively lower rate of 3.7%. It’s like Medicare Advantage plans have a special talent for denying claims. Maybe they should get an award for it.
But it’s not just the denial rates that make this problem so frustrating. The challenges in applying correct patient status are equally exasperating. Physicians and case managers have to deal with considerable subjectivity when it comes to determining whether a patient should be admitted as an inpatient, outpatient, or observation. It’s like they’re playing a never-ending game of “Guess the Patient Status.” How exciting!
And let’s not forget about the financial impact on healthcare organizations. In 2021, hospitals wrote off a whopping 3.6% of their inpatient revenue as uncollectible. But wait, it gets better. In 2022, that percentage jumped to a staggering 5.9%. It’s like hospitals are throwing money out the window while simultaneously doing the cha-cha with denial letters. What a dance party!
With denial rates soaring and financial sustainability at risk, it’s clear that something needs to change. And that’s where artificial intelligence (AI) swoops in like a superhero in a shiny cape. AI can provide real-time data insights into each patient’s clinical picture, helping to eliminate the subjectivity in determining patient status. Goodbye, “Guess the Patient Status” game! Hello, objective decision-making!
But AI doesn’t stop there. It also helps align providers and payers for appropriate care. No more battles between them over what constitutes medical necessity for inpatient care. It’s like AI is playing referee and saying, “Hey, let’s find some common ground, shall we?” Such a peacemaker!
And let’s not forget about the importance of improving clinical documentation and revenue integrity. AI can help healthcare organizations track patient progress in real time and in the context of the optimal geometric mean length of stay. It’s like having a crystal ball that tells you exactly when a patient is ready to be discharged. Abracadabra!
So, with the help of AI, healthcare organizations can prevent denials, improve revenue integrity, and enhance patient care and outcomes. It’s like turning a gloomy denial party into a joyful celebration of appropriate reimbursement. Who doesn’t love a good party, right?
In the next section, let’s delve deeper into how AI-driven analytics can further prevent denials and optimize productivity in healthcare. Brace yourselves for more AI awesomeness!
The Role of Artificial Intelligence (AI) in Denials Management
Artificial Intelligence (AI) has emerged as a game-changer in addressing the rising problem of healthcare denials. With its ability to provide real-time data insights, AI offers a promising solution to the challenges faced in applying correct patient status. No more relying on subjective assessments by physicians or case managers, as AI brings in objective and evidence-based decision-making.
One of the key advantages of AI in denials management is its ability to align providers and payers for appropriate care. By continuously evaluating each patient’s profile against a vast database of relevant cases, AI can generate highly precise predictive analytics. These analytics not only facilitate the determination of the most appropriate level of care but also ensure that healthcare organizations receive the rightful reimbursement.
Moreover, AI plays a vital role in improving clinical documentation and revenue integrity. With its ability to track real-time data such as lab results, vital signs, and physician orders, AI ensures that clinical documentation is accurate and up-to-date. This not only helps in avoiding denials but also safeguards the financial sustainability of healthcare organizations in the long run.
But let’s be honest here, the traditional approach of manual workflows and subjective evaluations was a real winner! Who needs efficiency and accuracy, right? We all love spending extra time on reviewing cases and dealing with denials. It’s so much fun!
In all seriousness though, AI is a significant step towards preventing denials by providing data-driven insights and improving collaboration between providers and payers. It’s time to leave behind the archaic methods and embrace the power of AI in healthcare.
So, are you ready to move away from the mundane and make way for a smarter approach to denials management? With AI by your side, you can say goodbye to the headache of dealing with denials and hello to improved patient care and outcomes.
In the next section, let’s explore how AI can help in preventing denials with its advanced analytics capabilities. But before that, take a moment to appreciate the effort it took to get here. Your stamina for reading is truly commendable! Kudos to you! Now, let’s dive deeper into the world of AI-driven analytics and revolutionize healthcare revenue integrity.
Preventing Denials with AI-driven Analytics
Statistics on denial rates:
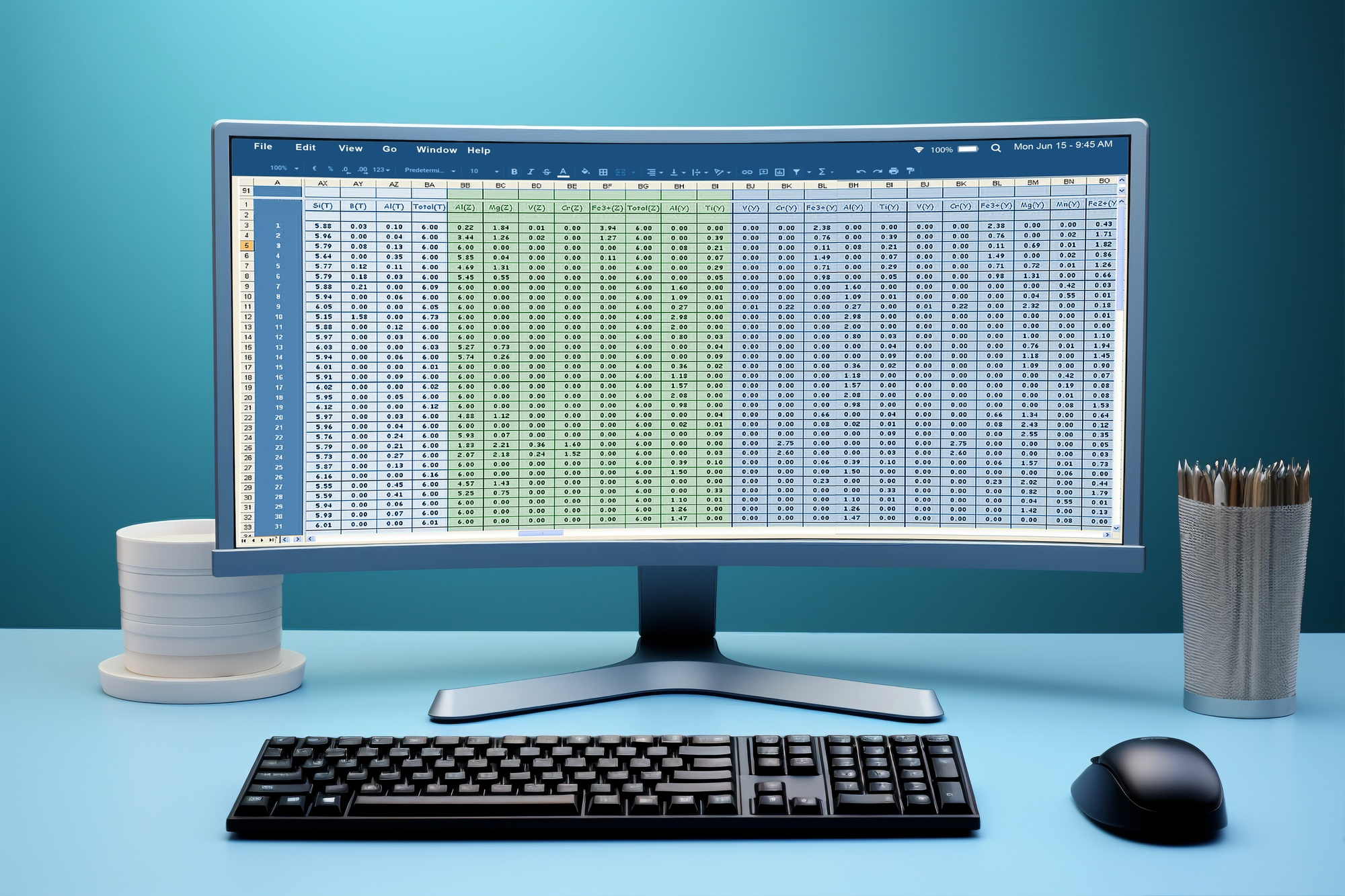
According to a recent industry survey, the initial inpatient level of care claim denial rate for Medicare Advantage plans was 5.8%, compared with 3.7% for all other payer categories. Hospitals participating in the survey wrote off 3.6% of their inpatient revenue as uncollectible in 2021, and that percentage jumped to 5.9% in 2022. It seems like denial rates are on the rise, and that’s not good news for healthcare organizations.
Challenges in applying correct patient status:
One of the main challenges in addressing denial problems is the considerable subjectivity in applying traditional inpatient admission criteria. Physicians and case managers often lack real-time data insights into each patient’s evolving clinical picture. This means they’re relying on outdated diagnosis codes or initial presentations that might change over time. Talk about a real headache!
The financial impact on healthcare organizations:
These denial issues create a perfect storm for healthcare organizations, jeopardizing their long-term financial sustainability. A recent survey conducted by the American Hospital Association (AHA) revealed that 89% of respondents experienced an increase in payment denials between 2017 and 2020. Half of the respondents even reported a “significant” increase in denials. Not exactly what you want to hear when your organization is trying to keep the lights on.
Outsourcing your billing can bring numerous benefits to your business, including increased efficiency, cost savings, access to specialized expertise, improved cash flow, the ability to focus on core activities, scalability, and enhanced data security. Consider partnering with a reputable billing service provider to optimize your billing processes and achieve better financial results.
Finding the right billing partner can be a daunting task, but fear not, my friend. Enter Wenour medical billing services, your ultimate solution to all your billing woes. With their expertise and years of experience in the field, they are the perfect match for your business. Say goodbye to the hassle of searching for a reliable partner because Wenour has got you covered.
Their team of billing experts will seamlessly integrate with your operations, ensuring a smooth and efficient billing process. From claim submissions to revenue cycle management, they’ve got it all under control. With Wenour by your side, you can focus on what truly matters – growing your business and enjoying that cup of coffee without any worries.
But that’s not all. Wenour takes pride in their commitment to accuracy and precision. They leave no room for error, diligently crossing every i and dotting every t. With their superhero-like attention to detail, you can rest assured that your billing is in safe hands.
So why wait? Take the leap and partner with Wenour medical billing services. They will revolutionize your billing process, saving you time, resources, and headaches. It’s time to embrace the freedom and peace of mind that comes with outsourcing your billing to the experts. Get ready to witness a new level of billing zen with Wenour by your side.
Conclusion
As we all know, healthcare denials have become quite the headache for many organizations. In fact, recent statistics show that denial rates have been on the rise, with hospitals experiencing a significant increase in payment denials. Don’t you just love it when your hard work gets denied? It’s like a slap in the face, isn’t it?
So, what’s causing this denial frenzy? Well, there are a couple of challenges at play here. Firstly, there’s the issue of subjective application of traditional inpatient admission criteria by physicians and case managers. It’s like they’re playing a guessing game with your health and finances. And secondly, the lack of standardization in clinical criteria used by payers just adds fuel to the fire. Can we all just agree on some rules and regulations, please?
But fear not, my friends, because artificial intelligence (AI) has come to the rescue! With its real-time data insights, AI can provide a much-needed solution to the denial problem. It helps align providers and payers for appropriate care, ensuring that patients receive the level of care they need without any unnecessary denials. Hallelujah!
And let’s not forget about the importance of good ol’ clinical documentation. With AI, healthcare organizations can improve their documentation processes and ensure that everything is accurately recorded. No more guesswork or missing information. It’s like having a personal secretary who never forgets anything. Lucky you!
But that’s not all folks! AI-driven analytics can also track patient progress and length of stay, helping healthcare organizations identify areas for performance improvement. It’s like having a personal coach who’s always pushing you to be better. You can do it!
And guess what? AI doesn’t just benefit the healthcare providers, it also enhances patient care and outcomes. By reducing denial rates and boosting revenue integrity, AI helps create a more efficient and effective healthcare system. It’s a win-win situation!
In conclusion, let’s all give a round of applause to AI for its incredible contribution to healthcare denials management and revenue integrity. With its real-time data insights, standardized criteria, and improved documentation processes, AI is revolutionizing the industry. So, let’s say goodbye to denials and hello to a brighter, more efficient healthcare future. Cheers to AI and all its wonders!