Tracking Lag Days: How Leading and Lagging Indicators Can Transform Your Practice

Leading and lagging indicators serve as pivotal tools in predicting future outcomes and evaluating past performances, respectively. Leading indicators, by identifying trends and patterns early, forecast future performance and signal potential issues before they escalate. Conversely, lagging indicators rely on historical data to offer insights into what has occurred, aiding in tracking progress with greater accuracy than their leading counterparts. Together, these indicators empower healthcare organizations to steer quality improvement and make strategic decisions more effectively. They analyze key performance indicators (KPIs), like emergency department wait times and surgical complication rates, to enhance patient care and operational efficiency.
Moving forward, this article will dissect the concept of lag days and its impact on healthcare practices, from financial performance to patient access. By scrutinizing strategies for minimizing lag days, integrating technology for better management, and emphasizing effective communication with insurance entities, the article aims to present a comprehensive guide on leveraging leading and lagging indicators. This exploration will not only highlight the importance of real-time feedback in improving team engagement and service recovery but also underscore the critical role that balanced scorecard metrics play in shaping cost-effective, patient-centered care. Through this lens, we will embark on a nuanced discussion on optimizing healthcare practices for superior outcomes.
Understanding Lag Days in Healthcare
Lag days in healthcare are defined as the interval between the date a service is provided and the submission of the corresponding claim to the insurance company. This delay can significantly impact the financial dynamics of healthcare facilities by creating uncertainties in revenue inflows. To mitigate these challenges, it is crucial for staff to enter their charges into the system within 24 hours from the service date.
The process of medical billing is intricate, involving several key steps: patient check-in, verification of insurance status, accurate medical coding, charge entry, claim submission, and finally, posting. Each stage must be executed efficiently to minimize lag days and enhance the revenue cycle.
Key Strategies to Reduce Lag Days
- Technological Integration: Implementing advanced technologies can automate many of the manual tasks involved in the billing process, thereby reducing the time between service provision and charge entry.
- Efficient Team Building: Developing a team skilled in swift and accurate charge entry is essential. Regular training and performance reviews can help maintain high standards.
- Process Review: Continuously analyzing and refining billing processes ensures that delays are identified and addressed promptly.
Charge Lag Metrics
Charge Lag, another critical metric in healthcare revenue management, measures the time from the date of service to when the charges are officially entered into the billing system. The industry standard for Charge Lag is ideally between 24 to 48 hours. To improve this metric, healthcare providers can:
- Implement charge capture technology to ensure that services are billed accurately and promptly.
- Conduct regular audits to identify and rectify discrepancies in the charge entry process.
- Provide ongoing training to staff to keep them updated on best practices in charge entry.
By tracking and optimizing these metrics, healthcare providers can significantly enhance their operational efficiency. For instance, Wenour, a leading medical billing company, offers specialized services that streamline charge capture and submission processes, effectively reducing lag days and improving financial outcomes for healthcare facilities.
Understanding and managing lag days is not just about improving financial performance but also about enhancing patient satisfaction by ensuring a seamless billing experience. As healthcare providers aim to optimize their operations, focusing on reducing lag days through strategic interventions and technological advancements remains a pivotal aspect of their financial health management strategy.
The Impact of Lag Days on Financial Performance
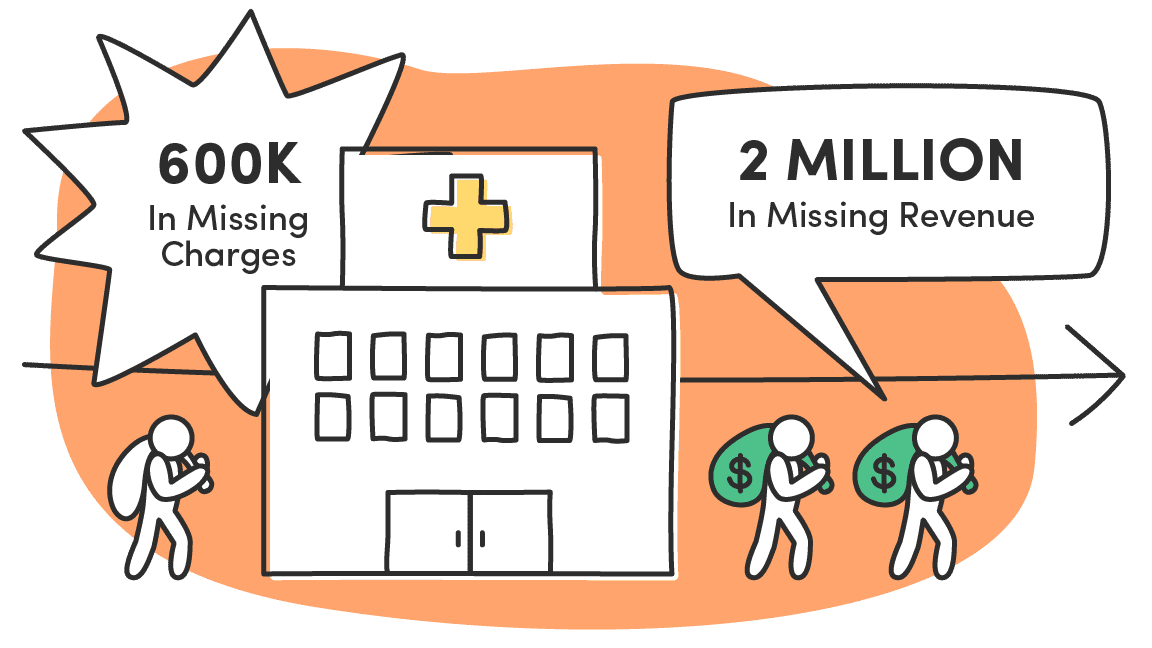
Minimizing lag days is crucial for enhancing the financial performance of healthcare practices. By reducing these delays, practices can see a significant improvement in their revenue cycle efficiency, leading to better financial returns. For instance, one hospital managed to reduce its lag days from 30 to just 10, which resulted in a remarkable 20% increase in income within a mere six months. This demonstrates the direct impact that efficient handling of lag days can have on a healthcare facility’s bottom line.
Furthermore, a shorter charge lag enables healthcare practices to bill for services more promptly, thus accelerating the reimbursement process. This is vital for maintaining a healthy cash flow, which is essential for the operational stability of any medical practice. By driving charge lag as low as possible, practices can achieve greater predictability in their cash flows, which in turn supports all aspects of their operations.
In addition to financial benefits, reducing lag days also contributes to the overall financial health of medical practices by streamlining operations and enhancing revenue streams. For example, companies like Wenour specialize in medical billing services that optimize charge capture and submission processes, effectively reducing lag days and improving financial outcomes for healthcare facilities.
Moreover, high-quality hospitals that effectively manage lag days may attract more patients through a better reputation or avoid negative financial impacts from programs like the Hospital Readmissions Reduction Program (HRRP) or other quality-based payment programs. These programs often impose financial penalties on facilities that do not meet certain standards, thus incentivizing hospitals to maintain efficient and high-quality operations.
By focusing on quality improvement, healthcare facilities not only enhance patient care but also reduce operating expenses. This is because quality improvements help avoid process inefficiencies, overuse, and preventable harms, all of which can lead to substantial cost savings. As such, the financial incentives to improve quality are considerable, further highlighting the importance of effective lag day management in healthcare practices.
Strategies for Reducing Lag Days
To effectively reduce lag days in healthcare, a variety of strategies can be employed, focusing on both technological advancements and process optimization. Here’s a detailed look at these strategies:
Utilize Modern Charge Capture Systems
Modern charge capture systems, such as those provided by pMD, offer significant reductions in charge lag. These systems enable instantaneous data entry, centralized access, built-in error checks, and robust data security, ensuring that billing is both accurate and timely.
Streamline Documentation and Coding Processes
It is critical that consults are documented, coded, and closed on the same day as the patient encounter to prevent delays. Similarly, procedural documentation should be completed immediately after the procedure ends, with coding and charge entry finalized by the end of the service date. This prompt processing ensures that documentation is readily available to backend staff, who should then code and prepare claims on the same day.
Harness Technological Potentials
Employing Electronic Health Records (EHR) or Practice Management Software significantly aids in scheduling appointments, documenting visits, and keeping patient data updated. This technology not only enhances submissions but also streamlines various processes across healthcare organizations.
Automate Billing Processes
Automating routine steps in the billing cycle can save time and increase efficiency. This allows medical billing staff to focus on addressing complications in filed claims, thereby reducing the overall time from service to bill submission.
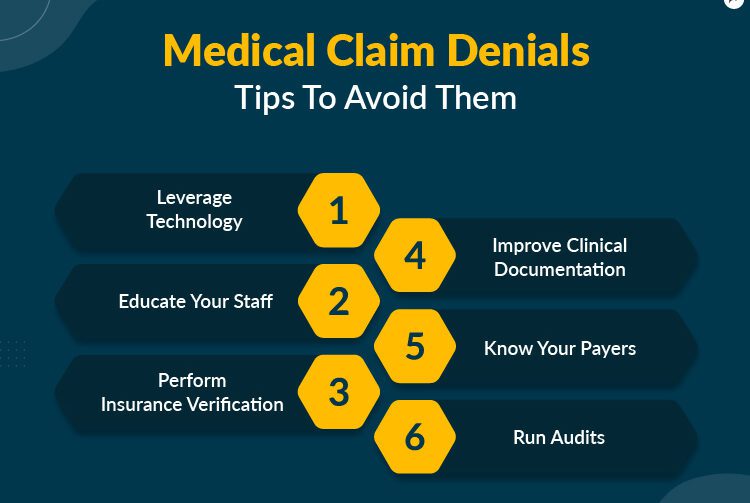
Proactive Management of Denied Claims
Following up on denied claims is crucial, as estimates suggest that as much as 50% of these claims are never revisited, leading to lost revenue. Effective practices include reexamining denials, prioritizing resolution, and correcting errors in claim submission or providing additional documentation as needed.
Build and Train Efficient Teams
Creating a team of experienced medical billing specialists and well-trained front-desk personnel is essential. Regular training and updates on changing laws, technological advancements, and industry norms ensure that the team remains effective and efficient.
Regular Process Reviews
Regularly reviewing processes helps identify drawbacks and enhances methods to keep up with current trends in the healthcare system. Encouraging staff to present growth ideas and having reports on financial and administrative processes are part of this strategy.
Implement a Rules-Based Quality Engine
Utilizing a rules-based engine for quality assurance ensures that all claims comply with coding guidelines before submission. This reduces the chances of denials due to coding errors.
Real-Time Eligibility Verification
Using real-time eligibility tools to verify coverage details before and at the time of service helps to curb charge lag due to issues with coverage and benefits.
By integrating these strategies, healthcare providers can significantly reduce lag days, enhancing both financial performance and patient satisfaction. Notably, companies like Wenour specialize in optimizing these processes, offering tailored solutions that streamline operations and improve financial outcomes for healthcare facilities.
Integration of Technology to Manage Lag Days
In the realm of healthcare, the integration of advanced technology plays a crucial role in managing and reducing lag days, which are critical for maintaining efficient revenue cycle management and enhancing patient care. Here is an exploration of various technological solutions that have proven effective in this domain.
Modern Technology Platforms and Systems
TheSNFist™ Suite Technology Platform
This comprehensive technology platform supports theSNFist™ Suite of services, providing real-time visibility into the revenue cycle. It enables practices to proactively manage lag days by offering tools that streamline the billing process and enhance data accuracy.
PacEHR™ Electronic Health Record
PacEHR™ is a fully integrated electronic health record system designed to support efficient and accurate documentation. By minimizing documentation errors and delays, this system plays a pivotal role in reducing lag days, ensuring that billing and medical coding are promptly addressed.
Point of Care Charge Capture
Utilizing a mobile app for real-time charge capture at the point of care significantly cuts down on lag days. This technology allows healthcare providers to immediately record charges, reducing delays typically caused by traditional charge creation processes.
SNFConnect Communication System
Effective communication is vital in healthcare settings, especially between different providers. The SNFConnect system facilitates seamless communication, which is crucial for reducing lag days that can occur due to delays in information exchange.
Automated Solutions and Business Intelligence
Comprehensive Medical Billing Software
Employing robust medical billing software automates repetitive tasks and streamlines the entire billing process. This not only reduces manual labor but also decreases the likelihood of errors, contributing to reduced lag days.
Business Intelligence Tools
Advanced analytics and business intelligence solutions, such as Power BI, provide live interactive reports that offer real-time insights into charge lag. These tools help measure charge lag, generate exceptions, and identify key contributors to inefficiencies, thus enabling targeted interventions.
Workflow Optimization Technologies
Low code or no code software solutions are increasingly being adopted in healthcare settings due to their user-friendly interfaces and reliability. These technologies streamline patient visits, reduce staff overhead, and improve clinical documentation efficiencies, which in turn decrease lag days.
Artificial Intelligence and Advanced Analytics
The use of AI-enabled analytics and expansive data sets facilitates a shift from traditional lagging indicators to more predictive, leading indicators. This transition is crucial for proactive management of healthcare practices and can significantly reduce lag days.
Specialized Billing and Customization Features
Practolytics offers specialized billing services for various medical fields, which is complemented by technology that allows for feature customization. This customization empowers the use of business intelligence and analytics tailored to specific medical billing needs, such as Spavato, urgent care, and oncology, among others.
By integrating these advanced technological solutions, healthcare providers can achieve a significant reduction in lag days. This not only improves financial performance but also enhances patient satisfaction by ensuring timely and accurate billing. Moreover, companies like Wenour specialize in optimizing these processes, offering tailored solutions that streamline operations and improve financial outcomes for healthcare facilities.
Optimizing Patient Documentation
Effective patient documentation is pivotal in enhancing healthcare efficiency and accuracy. Here are several strategies to optimize this crucial process:
Point of Care Documentation
Point of care (POC) charting, which involves recording patient information directly at the bedside, significantly boosts documentation accuracy and efficiency. This method ensures that patient data is captured and updated rapidly, maintaining comprehensive medical records. By improving access to critical patient information, POC charting facilitates better communication and decision-making among the healthcare team. Additionally, real-time documentation at the point of care minimizes errors caused by delayed data entry, thus preserving the integrity and authenticity of Electronic Health Records (EHRs).
Enhancing Electronic Health Records (EHRs)
To further enhance patient documentation, healthcare providers should focus on accurate and comprehensive data entry in EHRs. Using standardized coding systems, workflows, and templates ensures consistency and compliance with regulatory standards. It is crucial to maintain data completeness by including all relevant patient information and regularly reviewing and validating this data for consistency and accuracy. Employing user-friendly dashboards and interfaces can reduce the time required for documentation, allowing healthcare professionals to spend more time on patient care.
Implementing Best Practices in Documentation
Healthcare organizations should adopt best practices such as using clear, accurate, and objective language in their documentation. Timely documentation is essential to ensure the availability of correct patient data in real-time. Standardized templates help align clinical documentation with specific norms and requirements, organizing and structuring clinical notes to reduce repetition and enhance efficiency. Additionally, leveraging advanced digital health technologies, such as telemedicine and artificial intelligence, can revolutionize healthcare practices by enhancing workflow efficiency and personalizing patient care.
Training and Compliance
Ensuring that all healthcare professionals are well-trained in the implementation of clinical guidelines is crucial. Various training strategies, such as creating groups of “super users,” can provide internal instruction to clinicians or office staff, enhancing the effectiveness of electronic documentation systems. Moreover, confidentiality must be rigorously maintained as per the Health Insurance Portability and Accountability Act (HIPAA), protecting all patients’ personal health information.
Collaboration and Customization
Encouraging teamwork and collaborative initiatives for data collection and validation is essential. Healthcare professionals should work together to resolve inconsistencies or gaps in documentation, with ongoing feedback and education provided to improve performance and skills. Customizing EHR features to meet the specific needs of different medical fields can also enhance documentation processes, as seen with companies like Wenour, which specialize in optimizing these systems for improved healthcare outcomes.
By integrating these strategies, healthcare providers can optimize patient documentation, thereby enhancing the overall quality of patient care and operational efficiency.
Effective Communication with Insurance Companies
Effective communication with insurance companies is pivotal in managing healthcare practices efficiently. Here are some strategies to enhance interactions and ensure smoother operations:
Be Clear and Concise
When dealing with insurance companies, it’s crucial to communicate in a straightforward manner. Avoid using jargon or overly technical language that could lead to misunderstandings or delays.
Maintain Professionalism Under Pressure
Remaining calm and respectful during conversations with insurance representatives is essential, even when faced with frustration or setbacks. This approach can lead to more productive interactions and quicker resolutions.
Understand Your Rights
Being well-informed about the insurance coverage, policy terms, and relevant laws and regulations is crucial. This knowledge empowers healthcare providers to advocate effectively for their needs and rights.
Document All Interactions
Keep detailed records of all communications with insurance companies. This should include the date, time, details of the conversation, and the contact information of the representative. Such documentation can be invaluable in resolving disputes or discrepancies.
Seek Professional Assistance When Needed
If resolution of billing or coverage issues becomes challenging, consider consulting external experts. Legal advisors, consumer advocacy groups, or specialized services like Practice Solutions can offer necessary guidance and support.
Escalate When Necessary
Do not hesitate to escalate the issue within the insurance company if initial attempts at resolution are unsuccessful. Sometimes, higher-level intervention may be required to address your concerns effectively.
Offer Multiple Communication Channels
Providing various channels for interaction can enhance the member experience, allowing them to choose their preferred method of communication. This flexibility can lead to improved satisfaction and engagement.
Personalize Interactions
Tailoring communications to the specific needs and circumstances of members can significantly increase engagement and satisfaction. This approach should also comply with ADA and Section 508 to ensure accessibility for all members.
Use Technology to Enhance Efficiency
Implementing advanced technology solutions can streamline communication processes. Automated systems and real-time data access can reduce delays and improve the accuracy of information exchanged.
Monitor and Adapt Strategies
Regularly assessing the effectiveness of communication strategies and making necessary adjustments based on feedback and industry trends is crucial. This proactive approach can help in maintaining high standards of service and member satisfaction.
By adopting these strategies, healthcare providers can improve their interactions with insurance companies, leading to better management of billing processes and enhanced patient care. Additionally, companies like Wenour specialize in optimizing these communication strategies, providing tailored solutions that enhance operational efficiency and financial outcomes.
Monitoring and Analyzing Lag Days Metrics
Effective monitoring and analysis of lag days metrics are crucial for healthcare organizations to enhance operational efficiency and patient care. Here, we explore the essential metrics and strategies for effective monitoring.
Key Performance Indicators (KPIs) in Healthcare
Healthcare KPIs serve as vital signs of an organization’s health, reflecting the current state of healthcare delivery and bolstering patient care and operational efficiency. These indicators are divided into leading and lagging indicators, each providing unique insights. Leading indicators, such as management leadership and worker participation, are proactive and help predict future trends, while lagging indicators, like the number or rate of injuries, offer valuable insights into past performance.
The Role of Leading and Lagging Indicators
Leading indicators in healthcare are proactive, preventive, and predictive measures that provide information about the performance of safety and health activities. They help healthcare providers anticipate trends, identify issues early, and adjust their strategies accordingly. On the other hand, lagging indicators measure the occurrence and frequency of events that occurred in the past and help healthcare practices evaluate their performance and ensure quality care.
Implementing and Utilizing a Balanced Approach
For effective metric monitoring, it’s crucial to implement KPIs in a healthcare setting following a deliberate and structured approach, starting with establishing clear objectives aligned with organizational goals. Organizations should avoid relying too heavily on one type of indicator and ensure staff are trained on correctly interpreting KPI data. Both leading and lagging indicators should be used together for the successful improvement of safety performance.
Real-Time Feedback and Data-Driven Decisions
Real-time feedback leads to team and patient engagement, allowing organizations to course-correct, provide service recovery, and expand positive behaviors. This approach enables healthcare providers to make data-driven decisions and positively impact patient experiences and outcomes. Additionally, acting on leading data can influence lagging indicators such as CAHPS, enhancing overall healthcare service quality.
Revenue Cycle KPIs and Dashboard Monitoring
Monitoring Revenue Cycle KPIs provides insights into operational efficiencies, revenue generation, and any repetitive losses incurred. Important metrics to include in a revenue cycle dashboard are Days in Accounts Receivable, Clean Claim Rate, and Charge Lag, among others. Tools like Databox offer free, personalized revenue cycle dashboards for healthcare businesses to monitor these KPIs in real time, helping identify areas where compliance risks are high and payment processing can be improved.
Specialized Services and Technology Integration
To further enhance the monitoring of lag days metrics, healthcare providers can consider partnering with specialized services like Wenour, which offers tailored solutions that streamline operations and improve financial outcomes. Integrating advanced technology platforms and systems can also play a crucial role in managing and reducing lag days, thereby maintaining efficient revenue cycle management and enhancing patient care.
By effectively monitoring and analyzing lag days metrics, healthcare organizations can not only improve their financial performance but also enhance patient satisfaction and overall care quality.
Conclusion
Through the comprehensive exploration of tracking lag days, the vital significance of leading and lagging indicators in healthcare has been underscored, revealing their paramount role in enhancing operational efficiency and patient care. By scrutinizing strategies from technological integration to optimizing patient documentation and fostering effective communication with insurance companies, the article has offered a holistic guide to mitigating lag days and enriching healthcare practices. Importantly, it highlighted how companies like Wenour specialize in streamlining these processes, which, in turn, augments financial performance and patient satisfaction – reinforcing the critical nature of balanced scorecard metrics and real-time feedback in the quest for quality improvement and cost-effective patient-centered care.
Harnessing the right medical billing services stands as a linchpin in navigating the complexities of healthcare billing and management, proving indispensable for healthcare providers aiming to reduce lag days and enhance financial outcomes. In this light, the integration of advanced technological solutions and effective strategies discussed herein casts a promising pathway towards not only achieving superior financial health but also elevating the standard of patient care across the healthcare spectrum. To take a stride toward optimized operational efficiency and patient care within your healthcare practice, explore the best medical billing services in the USA. Together, these efforts underscore a collective movement towards a more efficient, patient-centered healthcare system.
FAQs
What are the advantages of utilizing both leading and lagging indicators? Leading and lagging indicators together offer a complete picture of a company’s performance. Leading indicators can be seen as the driving forces that inform proactive actions to meet goals, while lagging indicators provide the measurable outcomes of those efforts.
How can leading and lagging indicators be applied to gauge performance effectively? To effectively gauge performance, it’s advisable to pair leading and lagging indicators within a specific strategic framework to monitor cause and effect relationships. For example, in a strategy aimed at boosting sales, the number of sales calls (a leading indicator) can be correlated with the total sales achieved in a certain timeframe (a lagging indicator).
In what way do leading and lagging indicators collaborate to enhance business outcomes? Leading indicators are predictive, giving insights into future performance, while lagging indicators offer a retrospective view on past results. Tracking both is crucial as they collectively aid in pinpointing areas for product and business enhancements.
Do leading and lagging indicators contribute to the effectiveness of safety practices? Yes, leading and lagging indicators are valuable for safety practices. Lagging indicators can signal a breakdown in safety protocols or the presence of a hazard, whereas leading indicators provide early indications of the effectiveness of safety measures in preventing incidents.